Hospital pricing, ambulances, and qualitative research
January 18, 2023
My cohort-mate Elodie Chervin, a tall Frenchwoman with a better American accent than mine, presented in December a paper she had worked on as a research assistant for Zach Cooper at Yale.The notebook with my notes from Elodie’s talk mysteriously disappeared in Mexico (not mysterious, it was stolen from a rental car after the back window was smashed in). And I’m not going to actually read the paper; grad students don’t have time for that. So this is mostly based on memory. The paper is called “Do Higher-Priced Hospitals Deliver Higher-Quality Care?,” and finds positive results, with a caveat for market concentration.
While higher-priced hospital services are better in areas with competitive markets, once the authors look at consolidated markets, the effect goes away.Or reverses? Don’t remember. There’s been a trend towards hospital mergers, larger “health systems,” and this is the bad guy. The path goes something like: mergers —> ↑ market consolidation —> ↓ competition —> ↑ prices, with no endogenous change in the level of care. So having higher prices makes you a better hospital (lol causality) in competitive markets, but there’s no reason for this to be true in consolidated markets.
There’s a graph which shows up often around people with an intellectual interest in inflation, like first-year microeconomics students or New York Times readers:
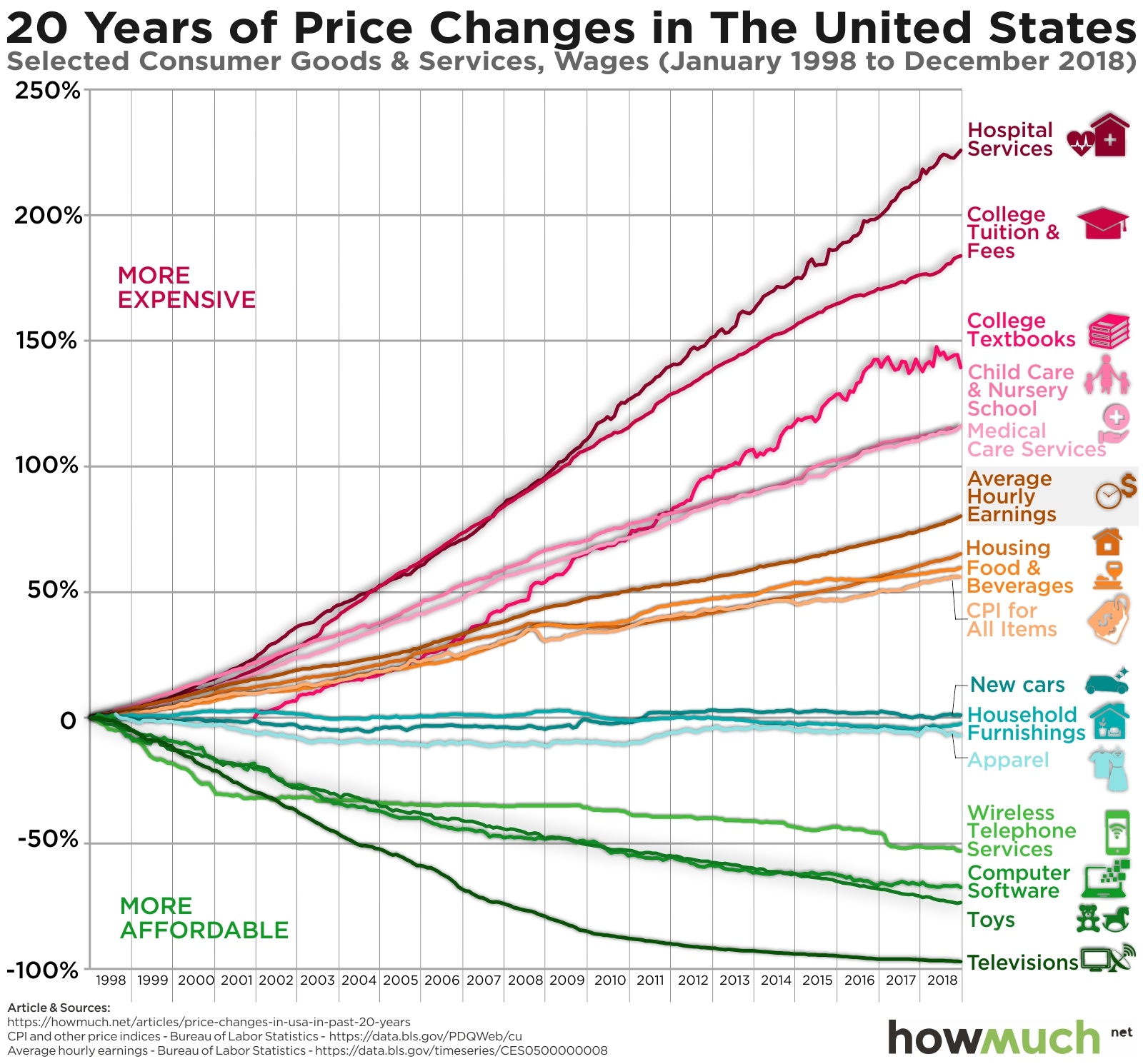
Also — I just bought a television in the UK! Wow are those things cheap.
The moral is, while it’s great televisions are getting cheaper, the “important” stuff is getting more expensive faster than wages, and the only goods which are getting cheaper are boring, opiate of the masses consumer goods.Another plausible story is about the Moore’s law as a black hole for innovation. We’ve gotten unspeakably good at cramming transistors onto a chip, but this innovation hasn’t (yet) spilled over to revolutions in the healthcare sector. I like this story more, but it’s not as relevant.
An aside — one of my soapboxes is the increasing fraction of for-profit nursing homes. Something like three-quarters of skilled nursing facilities (SNFsThere are many jokes about ‘sniffs’ among EMTs, with numerous possibilities of what the ‘S’ could stand for. ) are for-profit, compared to one-third of hospitals. One example which has made my life sadder and smellier is HCR Manorcare, a chain of SNFs which Carlyle acquired in a messy LBO 20 years ago. I don’t have any evidence that PE-run SNFs are worse than privately owned facilities… oh wait, yes I do:
PE ownership increases short-term mortality by 13% and reduces other measures of patient well-being, while also increasing revenue per patient by 10%. Clinical and operational changes help to explain these effects, including declines in nursing staff and lower compliance with care standards.
This is a great paper — there’s a cool instrumental variables approach to deal with changing patient composition. And it brims with righteous anger: the authors aren’t afraid to write that their results imply “20,150 lives lost due to PE ownership over our twelve-year sample period.” Now, I’m slightly equivocating between PE-run and privately owned SNFs.
Back to Elodie’s work: to identify the effect of a hospital’s care on patient outcomes, they used the preferences of ambulance companies towards certain hospitals. These preferences are unrelated to patient characteristics, so which hospital any individual patient goes to is plausibly exogenous.My favorite phrase in applied econometrics. This is a fantastic identification strategy.It’s not original to this paper — Doyle et al. (2015) first used this IV strategy, and it’s becoming more widespread. Ambulance services, especially private ambulance companies, are messy and chaotic in just the right amount to give the authors a paper.Another member of my cohort, Daniel Barbosa, has been presenting a paper on police body cameras in Brazil with a similar identification strategy. If one of the other six of us can put together a paper on plausibly exogenous assignment of firefighters, we’ll have the trifecta.
By the end of the talk, I had a dozen questions written down for Elodie about ambulance data and the assumptions the research team made: how to deal with consolidation of ambulance companies? When ambulance crews bid for calls,While often the nearest ambulance is dispatched, these systems aren’t perfect, and other ambulances can assign themselves if they think they’re closer or can provide better care. This also leads to some companies or crews ‘assigning’ themselves more serious patients. are those patients treated as less randomly assigned? Do they control for the quality of the snacks in the emergency room?Mutatis mutandis, an arbitrary ambulance crew would prefer to bring a patient to Shady Grove Adventist Hospital than Suburban Hospital, because SGAH has Nutri-Grain® bars. Did the team have data on patient hospital preference?
I didn’t get to ask all of these questions, but the last one gets to my largest concern with the Cooper et al. identification strategy. Getting someone onto an ambulance presents two types of challenges. First, the physical: by definition, our patients are unfit. We have many contraptions to lever, lift, or lug patients into these very expensive minivans, but patients can always find ways to make it more exciting and difficult. The second type of challenge is conversational. So many people call an ambulance despite not wanting to go to the hospital at all, and that’s aside from all of the 911 calls made against the will of the patient.
A large portion of this reluctance is not towards hospitals per se, but hatred of some specific institutions, or attraction to others. By default, ambulances in most states are directed to “the closest appropriate facility,” and as there isn’t that much differentiation between hospitals capabilities on paper,Here, I just mean that every hospital with an emergency room can take almost all ambulance patients. The edge cases are things like pregnant women who have suffered a traumatic injury, or burn patients, who can only go to certain facilities. this really means “closest facility.” Patients don’t want to go to the closest facility, they want to go to the hospital where they visit their primary care provider, or the nice Catholic hospital 25 miles away, or anywhere but [REDACTED].
This leaves ambulance crews with a very strong rhetorical tool: “shut up and get on the damn stretcher, and we’ll take you wherever you want to go.” This presents the econometricians among us with a problem: if patients can choose which facilities they want to go to, ambulance companies no longer gives us a plausibly exogenous hospital assignment.
Thankfully this is answerable with the data. On the patient reporting system used byAt least the two systems I’m familiar with; some googling shows that these two providers have a majority of the market share in the US ambulance crews, there’s a field for “reason for destinationI.e., why are we going to this hospital choice.” For >95% of the patients I’ve transported, I selected one of just two answers: “Closest Facility” or “Patient’s Preference.” It’s possible that patient preferences have a negligible effect on their final destination. But if this is a problem, the data offer another way out. By focusing only on patients whose preferences don’t fuck with the quasi-random assignment to hospitals, we could recover our identification strategy!
Do I actually think this dooms the Cooper et al. identification strategy? Probably not. The effect of patients’ preferences would be more distortionary in less consolidated markets, as patients there would have more facilitiesIn less consolidated markets, facilities are also more differentiated, leading to stronger preferences. to choose between. So the effect would be in the same direction as the increase in competition and decrease in prices observed by Cooper.Lots of spitballing in this paragraph. Things are more complicated than this.
Branko Milanović is a delightfully contrarian and crotchety economist; his work on inequality is important and well-written. Listening to Elodie’s talk, one of Milanović’s old blog posts came to mind:
Recently I read, rather by accident than design, short lives of several contemporary economists. What struck me was their bareness. […] How can people who had lived such boring lives, mostly in one or two countries, with the knowledge of at most two languages, having read only the literature in one language, having travelled only from one campus to another, and perhaps from one hiking resort to another, have meaningful things to say about social sciences with all their fights, corruption, struggles, wars, betrayals and cheating. Had they been physicists or chemists, it would not matter.
[…]
Faced theoretically with a given problem, we can provide a perfectly reasonable and coherent answer and even explain well the choices. But then, if faced by the same problem in our own lives, we shall quickly find out that such well-reasoned answer was only partially correct. It failed to take into account a number of secondary issues, many conditions and constraints that, in the abstract case, we either ignored, assumed away, or most likely just never thought about. Or never imagined.
Obviously, you can do good economics research while living a “boring” life.Unlike Milanović, I don’t particularly want economics professors who ‘had to drink poison to make a point (Socrates), or were jailed and tortured (Machiavelli), or were executed on the orders of a national assembly (Condorcet), or banished and killed by a totalitarian regime (Kondratieff); or those who had to flee their governments and reinvent themselves (Marx), or move into incendiary politics (Weber), or migrate to another language and continent (Schumpeter, Hayek, Kuznets, Leontieff), or experience the thrill of forbidden pleasures (Keynes).’ And relative to most of my economist-y friends, I’m pretty far along towards the quantitative end of the axis. But qualitative, anthropological, field research in economics is neglected. Joseph Doyle, at MIT, wrote the first paper to use the ambulance identification strategy I described above — if he wanted a ridealong with Boston EMS, we could have hooked him up!It’s possible he or another co-author did take a ridealong, in which case this blog post is useless and you should ignore me. If Doyle had heard a grandmother arguing that she needs to go to Tufts and not BMC because her cardiologist is at Tufts, and if he had seen the look on the face of the paramedic who hadn’t slept since Wednesday, his identification strategy would have been strengthened. The paper would have survived learning about what it means for an ambulance to take a patient to a hospital. In econometrics, we’re nudged towards thinking of this as just another DGP,A silly acronym I’m purposefully not spelling out. but this process is messy and full of assumptions.
My favorite example of qualitative research by economists is a paper by Acemoglu, Reed, and Robinson in the JPE. The paper is called “Chiefs: Economic Development and Elite Control of Civil Society in Sierra Leone,” and is well-cited in the institutional development literature. Supplementing the paper, however, is a gorgeously comprehensive history of the chiefdoms of Sierra Leone, written (but never published) by Reed and Robinson. Tristan Reed, who’s now at the World Bank, spent two years as an RA wading through archives in London, Freetown, and Kenema. The data he uncovered made the JPE paper possible, but if these data had been accessible without traveling to Sierra Leone, and without learning the stories of the chiefdoms, it would have been a weaker work.
The Cooper et al. paper is really cool, and I’m glad I got to see Elodie talk about it! There should be more papers about emergency care. The UK is having it’s own ambulance-based crisis at the moment.
I’d like to write something more about this soon, and will link to it here if I do.